NHS Medical Doctor Degree Apprenticeship - All Facts in 1 Place


Find the latest info about the details, reasoning, requirements, vacancies and application process behind the Medical Degree Apprenticeship in one place.
Table of Contents
- 1 Understanding the Medical Apprenticeship Programme
- 2 Where Does the General Medical Council Stand on Medical Apprenticeship Programmes
- 3 What are Doctors Saying About the Medical Apprenticeship Programme?
- 4 Medical Apprenticeship Reviews
- 5 Potential Pitfalls of the Medical Apprenticeship Programme
- 5.1 Regulatory Challenges
- 5.2 Limited Entry Pathways
- 5.3 Intense Time Commitment, Stress & Potential Burnout
- 5.4 Training Quality and Consistency
- 5.5 Potential Shortage of Training Spaces
- 5.6 Limited Prestige and Recognition
- 5.7 High Workplace Pressure
- 5.8 Potential Long-Term Impact on the Workforce
- 5.9 Will Apprentices Have the Same Employment Opportunities as Traditionally Trained Doctors?
- 6 Join Our Webinar
- 7 What Viable Alternatives are there to Studying Medicine in the UK?
- 8 Conclusion
- 9 Q&A Medical Apprenticeship Programme
- 9.1 1. What is the Medical Apprenticeship Programme?
- 9.2 2. What does the General Medical Council (GMC) say about the programme?
- 9.3 3. How was the Doctor Apprenticeship Programme initiated?
- 9.4 4. What are the entry requirements for the Medical Apprenticeship Programme?
- 9.5 5. What does the training structure look like for apprentices?
- 9.6 6. What are the potential challenges of the Medical Apprenticeship Programme?
- 9.7 7. How is the programme perceived by current medical professionals?
- 9.8 8. Are there guarantees of employment upon completion of the apprenticeship?
- 9.9 9. What are viable alternatives to studying medicine in the UK?
- 9.10 10. How do you apply for a Medical Apprenticeship Programme?
It is no secret that the National Health Service (NHS) in the UK has been struggling with an increased demand for healthcare services, stretched resources, and staffing shortages. This has led to longer waiting times than usual and a pressing need for sustainable solutions to ensure quality care for the citizens of the United Kingdom.
To address this need, the Medical Doctor Degree Apprenticeship has been introduced as an experimental initiative. In essence, it is a programme that will allow students to receive paid training while studying to become a part of the NHS workforce.
In this comprehensive guide, we will give you all the available details about the Medical Apprenticeship Programme, including the application process, what the NHS hopes to accomplish, GMC’s stance on the programme, what current doctors in the UK are saying about it, and the potential associated negatives.
Please keep in mind that the information in this blog is accurate as of 19.04.2024 but is subject to change.
Understanding the Medical Apprenticeship Programme
The Doctor Degree Apprenticeship aims to address the shortage of medical professionals in the country by providing a non-traditional pathway into the medical profession. Its primary objective is to expand the future medical workforce and enhance diversity by recruiting individuals from a wider pool within local communities.
The Medical Doctor Degree Apprenticeship is designed to allow individuals to study to become physicians while working and earning a salary. This means that apprentices will get a university education while being employed by an NHS trust (an organisational unit that provides healthcare services within the NHS).


How the Doctor Degree Apprenticeship Programme Started
The Medical Apprenticeship Programme is a government initiative that was introduced by NHS England. In July 2022, the Institute for Apprenticeships and Technical Education (IfATE) and the Department of Education approved the medical doctor degree apprenticeship standard and outlined the requirements for apprentices.
To establish the programme, employers and medical schools received support from Health Education England, which is now part of NHS England. Their collaboration resulted in the development of the apprenticeship framework and the establishment of teaching standards for it.
In January 2023, the NHS confirmed pilot funding for the programme as part of a broader plan to expand the training of healthcare workers.
The Application Process for the Medicine Apprenticeship Programme
The first medical doctor degree apprenticeship application round for the pilot scheme was conducted in the Spring of 2024. It was done on a local scale through ‘closed information seminars’ or ‘screening/information events’, where prospective candidates were assessed. These closed application processes were carried out by the respective universities that will host the apprentices.
The first cohort of 200 apprentices is expected to start in September 2024. As of the information available, there are no medical doctor degree apprenticeship vacancies. However, due to the nature of the ‘closed’ applications, we do not have access to information from every medical school offering these programmes.
As of now, detailed information about the application process for the Doctor Degree Apprenticeship in future years is not explicitly outlined, due to the uncertainty of the programme. However, it is reasonable to expect a similar application process to the one carried out in 2024.
Medical Doctor Apprenticeship NHS Entry Requirements
The medical doctor degree apprenticeship entry requirements are similar to the typical rigorous prerequisites to study medicine. However, since each university has its own application process and each apprentice will be employed by a different NHS trust, requirement discrepancies can come up.
Generally, prospective apprentices will need to:
- Have high A-level grades in sciences, such as Biology and Chemistry. Some universities may also ask for Mathematics and Physics
- Have strong grades in GCSEs with ESFA-approved Maths and English Level 2
- Participate in an interview
Both the employing NHS trust and the medical school will set additional requirements. These prerequisites may include:
- Access to Medicine’ or ‘Access to Science’ course achieved within the past 5 years (30 Distinction & 15 Merit)
- 2:1 or above in a university-approved Science or Allied Health degree achieved within the past 5 years
- 2:1 or above degree in a non-Science/Allied Health subject with either of the following achieved within 5 years: A Level in either Biology, Chemistry or Physics A-Level (B grade or above)
- Additional assessments of the candidate's capability for academic learning and evaluations of their personal qualities, interpersonal skills, and behaviours suitable for a medical career.
Upon graduation, apprentices will need to meet all criteria set out by the General Medical Council (GMC). This includes passing the UK Medical Licensing Assessment (UKMLA) to qualify as a doctor.
It is important to note that the GMC has not yet approved any apprenticeship programmes, as stated in the following request from the Freedom of Information Act (FOIA).
Medical Apprenticeships Programme Structure
An apprenticeship will typically last 5-6 years, similar to studying for a bachelor’s degree in medicine. In the beginning, apprentices will spend most of their time (about 2/3rds of the year) learning at their respective universities, combined with working at their local NHS trust. Gradually, university hours will be phased out by hospital placements, followed by an induction for practice and shadowing a doctor.
A Cambridge-based medical university, which will be collaborating with the East Suffolk and North Essex NHS Foundation Trust, has published the following structure for its apprenticeship programme (*may be subject to change):
Total weeks of teaching for every year
| Year | University Teaching |
|---|---|
| 1 - 50 weeks | 33 weeks |
| 2 - 48 weeks | 30 weeks |
| 3 - 48 weeks | 24 weeks |
| 4 - 52 weeks | none |
| 5 - 43 weeks | none |
Hospital placements for every year
| Year | Hospital/GP Placements |
|---|---|
| 1 - 50 weeks | none |
| 2 - 48 weeks | 2-week hospital placement, 1-week GP placement |
| 3 - 48 weeks | Three 4-week rotational placements |
| 4 - 52 weeks | Nine 4-week rotational placements, incl. 1-week induction |
| 5 - 43 weeks | Five 4-week block placement, 4-week fixed SSC block |
Exams & work duration for every year
| Year | Exams | Work |
|---|---|---|
| 1 - 50 weeks | 2 weeks | 15 weeks |
| 2 - 48 weeks | 2 weeks | 13 weeks |
| 3 - 48 weeks | 2 weeks | 10 weeks |
| 4 - 52 weeks | 2 weeks | 8 weeks |
| 5 - 43 weeks | 3 weeks | 11 weeks |
Other activities for every year
| Year | Other Activities |
|---|---|
| 1 - 50 weeks | none |
| 2 - 48 weeks | none |
| 3 - 48 weeks | none |
| 4 - 52 weeks | 6-week elective placement |
| 5 - 43 weeks | 3-week ward simulation & induction for practice, 2 weeks foundation shadowing |
The curriculum is very rigorous and time-consuming with an average of 48 weeks of the year being dedicated to studying or working. Efficient learning skills, as well as stress and fatigue-management will be absolutely essential for any aspiring apprentice.To compensate for this busy schedule, apprentices will be entitled to annual leave.
Medical Doctor Degree Apprenticeship Salary
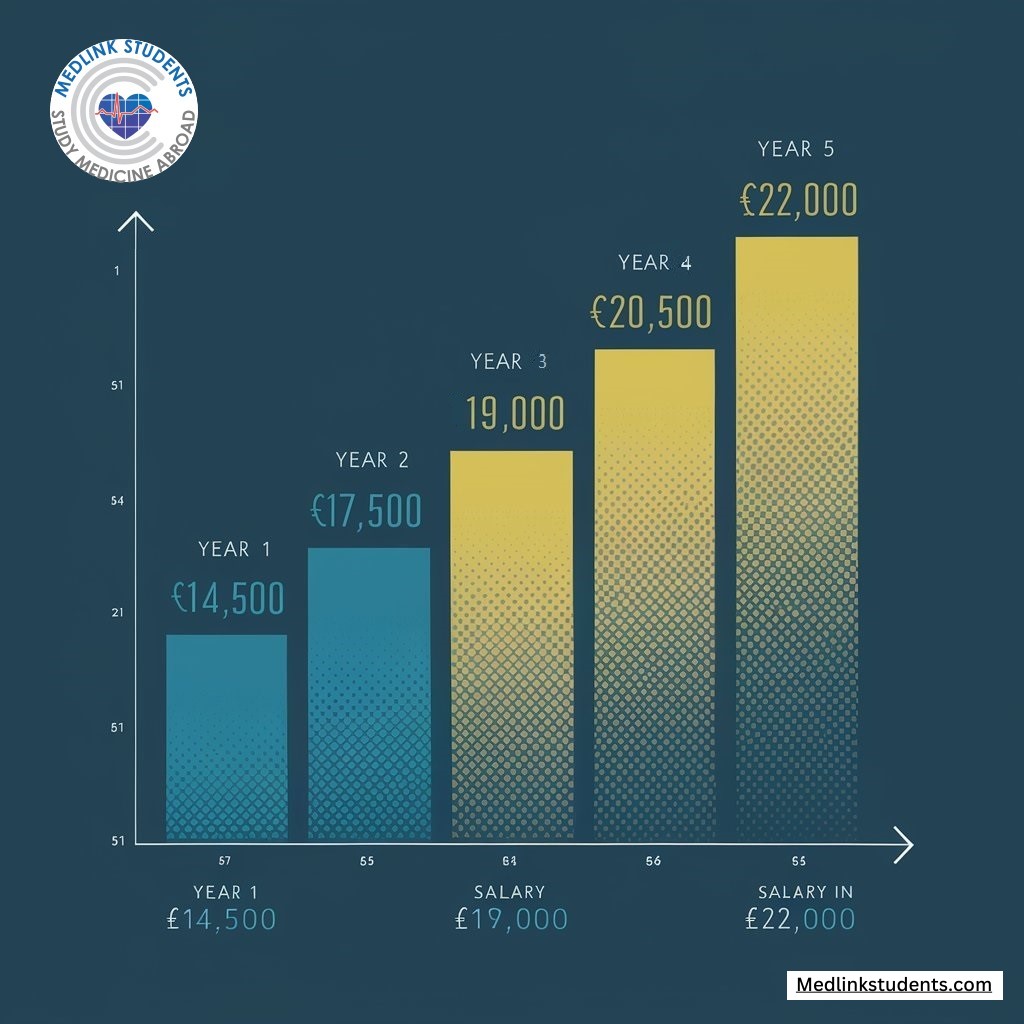
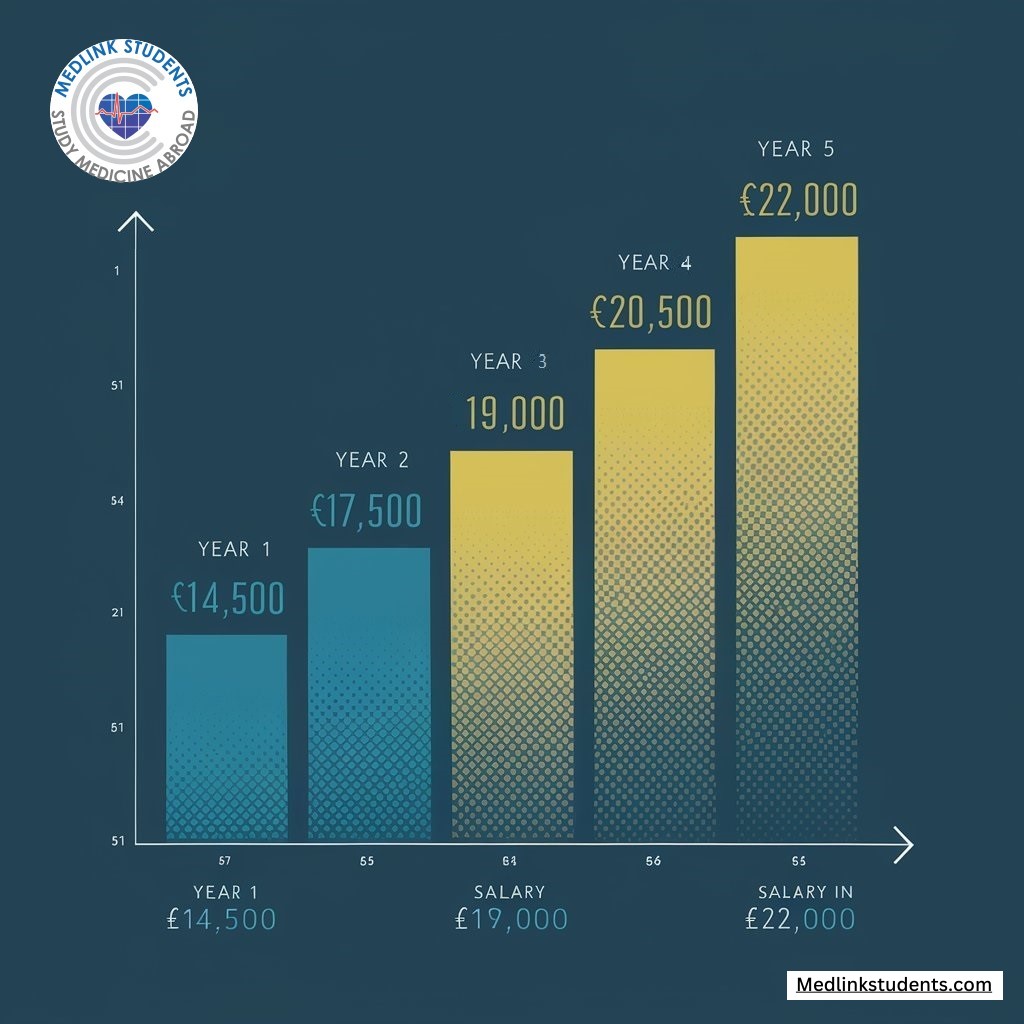
The stand-out feature of the Medicine Apprenticeships is that students will be earning a salary that increases year on year. Generally, apprentices can expect to earn around:
- Year 1: £14,500
- Year 2: £17,500
- Year 3: £19,000
- Year 4: £20,500
- Year 5: £22,000
However, it is crucial to note that payment amounts depend on the area and NHS trust where the apprentice will be working. These figures should only be taken as an example baseline that is subject to change.
Where Does the General Medical Council Stand on Medical Apprenticeship Programmes
A Freedom of Information Act (FOIA link) request to the GMC revealed the following:
- Quality Assurance: The GMC is not responsible or related to the operational aspects of the Apprenticeship Doctor Degree. However, it has the role of ensuring that any medical qualification, including those from apprenticeship programmes, meets their standards of quality and safety through their quality assurance processes.
The GMC’s reply is dated 15.03.24, and as of then, no apprenticeship programmes have been approved. - International recognition: The responsibility of gaining recognition from overseas medical councils lies with NHS England and the pilot medical schools.
So far, the international recognition of these programmes has not been addressed, and no medical councils have recognised them. - Career prospects: According to the GMC’s response, apprentices should have the same career opportunities as graduates from traditional pathways into medicine.
Due to the experimental nature and early stage of the apprenticeship programme, many aspects regarding recognition and career development are still unclear. Hence, many students and medical professionals have expressed their concerns about these uncertainties.
What are Doctors Saying About the Medical Apprenticeship Programme?
The medical degree apprenticeships have received mixed responses from medical professionals in the UK. While some express optimism that this could help alleviate some of the stress that is put on the healthcare system, many doctors remain uncertain and sceptical.
Medlink Students Interview with Dr. Philip Xiu
Dr Philip Xiu is an active part of the NHS in Leeds as a GP, a GP trainer, and a supervisor of the GP registrars in practice. He graduated from Pembroke College at the University of Cambridge with a Triple First Class degree and has also completed a Masters in Clinical Education at the University of Edinburgh. Additionally, he is the editor-in-chief of ClinicalKey Student, a crash course series editor, and the Chief Medical Officer at Medicalchain.
His achievements and deep understanding of the NHS training system make him the perfect choice to address the Medical Apprenticeship Programme. Here are his opinions and insights on the topic:
1. What is your General Opinion on the Medical Doctor Degree Apprenticeship Programme?
The Medical Doctor Degree Apprenticeship Programme is an innovative and ambitious endeavour that certainly comes with its sets of potential benefits and drawbacks. On the one hand, it stands to broaden access to the medical profession, which is a commendable goal given the financial and social barriers many potential candidates face. This could lead to a more diverse workforce that more accurately reflects the population it serves.
On the other hand, its impact on the medical profession and the quality of patient care hinges significantly on its execution. It's a delicate balance, ensuring that the program upholds the rigorous standards of medical training essential for patient safety and quality care. It's too early for anyone to predict its overall impact, but maintaining high educational and training standards will be critical.
2. Quality of Training Comparison
The apprenticeship model introduces an interesting dynamic in medical education by embedding students directly into the healthcare environment from an early stage. This practical exposure is invaluable, yet the consistency of the training experience could be a matter of concern.
Medical education relies heavily on a standardised curriculum to ensure comprehensive training, especially with the new UKMLA exam. Variations in training experiences and resources across different NHS trusts might challenge the educational outcomes for these apprentices. The NHS Trusts are already stretched with the increasing numbers of medical students and allied health professionals taught on the wards. The success of this model will likely depend on robust accreditation and monitoring systems to ensure each apprentice receives a quality educational experience that is on par with traditional pathways.
3. Addressing Workforce Shortages
The apprenticeship programme could play a role in alleviating healthcare workforce shortages, particularly by creating additional pathways into the profession. By potentially fast-tracking the entry of motivated individuals into the workforce and targeting training in high-need areas, the programme might offer a strategic response to localised shortages.
However, it's one piece of a much larger workforce puzzle. Addressing systemic issues such as retention, work-life balance, and job satisfaction among current NHS staff is equally critical to sustainably solving workforce challenges.
4. Challenges for Apprenticeship Route Students
Students choosing the apprenticeship route may encounter unique challenges, including managing the dual demands of work and study, which could extend beyond the challenges faced by traditional medical students. This is more so when balancing life, and also relationships.
Additionally, the varying quality of training across NHS trusts could impact their learning experience. Ensuring equitable access to a broad range of learning opportunities and clinical exposures will be vital. There's also the potential challenge of apprentices feeling fully integrated into the medical community, given the novel nature of their training path.
5. Doctors Taking on Apprentices
For doctors, the added responsibility of mentoring apprentices within their already demanding schedules could indeed prove challenging. It's imperative that this program does not inadvertently detract from patient care or the learning experience of existing medical students.
However, with proper planning, support, and resources, integrating apprentices could enrich the learning environment and provide valuable teaching experiences for doctors.
The key will be ensuring that these changes are implemented in a way that upholds the quality of care and enhances the training environment for all involved.
Fill in this form if you want a free consultation about better options for you, including studying medicine in Europe in English:
Check your email to Book a FREE call
with an expert advisor
Look at your promotions/spam folders, just in case.
Additional Expert Opinions on Medical Degree Apprenticeships
It’s essential to create a complete picture of the challenges that apprentices may face during the course of their programme and post-graduation. In this section, we will provide direct opinions and insights from a variety of medical experts and practitioners in the UK.
Here are the most common concerns regarding the Doctor Degree Apprenticeship Programme:
- The quality of the programme and whether it is sufficient to train qualified medical professionals
Doctors Association UK (DAUK) voted unanimously to oppose the scheme' due to reports that it would have a heavy primary care focus’. The association warned that GP trainers would not have the time to train apprentices adequately.
In the following Pulse article, the DAUK chairman, Dr Jenny Vaughan, questions the necessity of introducing such a programme at all. It can create a separate pathway into medicine, and it is ‘unlikely that the same levels of competence will be achieved.’ This poses a risk to apprentices, as they might be seen as less qualified than graduates who have gone through the traditional path of studying medicine.
She further stressed that the consultants and GPs who provide most of the clinical teaching are already under significant strain. Due to the heavy focus on primary care, the DAUK questions whether the NHS will have the capacity to supervise trainees.
DAUK GP Advisor Dr Lizzie Toberty has added that: ‘this apprenticeship scheme risks spending a lot of time and money to develop inadequately trained doctors. Without a thorough and rigorous grounding in the sciences, we risk dumbing down our health system. If patients do not have access to doctors with adequate clinical knowledge, their treatment will suffer.
- The financial and operational strains that will be put on the NHS
Additional concerns were raised by the British Medical Journal (BMJ) about whether current medical professionals will be able to take on apprentices at all and if this untested programme will provide adequate training. The NHS workforce is already under significant stress, as currently, the UK needs 50,000 new doctors to meet the EU average number of doctors per capita.
It isn’t clear whether doctors will have sufficient time to properly train apprentices to become a competent part of the NHS. There is also uncertainty about whether apprentices will be able to contribute enough to the workforce during their apprenticeship to justify the resources invested in their training. - Is it ok for applicants to join the workforce if they didn’t make it into medical school?
In an interview with the DailyMail, Dr Martin Scurr, a retired GP and Good Health columnist, expressed concern that the scheme ‘could create a second-class cadre of doctors'. This raises the question of whether graduate apprentices will be treated with the same level of respect as traditionally trained doctors or if they will be seen as less qualified.
Additionally, Barry Paraskeva, a consultant surgeon at Imperial College NHS Trust in London, questioned whether the apprentices would be as academically equipped as those who have gone through the traditional medical school route.
His doubts highlight the important question about apprentices' preparedness, which underlines the need for a curriculum that fully prepares them not only practically but also academically. Standardised quality assurance is needed to ensure that apprentices are on par with their traditionally educated peers.
Medical Apprenticeship Reviews
As this programme is still in its early stages, there aren’t any formal reviews yet. However, we’re closely monitoring developments and will update this section with feedback and insights as they become available.
Potential Pitfalls of the Medical Apprenticeship Programme
While apprenticeships introduce an untraditional path into the medical field, it's essential to understand some of the significant challenges that prospective students and the UK medical community may face with this non-traditional approach:
Regulatory Challenges
The programme is still very young, and there are many uncertainties regarding the recognition of qualifications, licensure, and certification, which could create obstacles for apprentices seeking to practise in certain regions or specialities.
Medical apprenticeships could significantly limit the options available to graduates, especially if they want to become doctors abroad. As qualifications and licensure under this scheme are still being defined, there is a real risk that these credentials may not be recognised internationally.
This could mean that once apprentices join the NHS workforce, they may become committed to it.
Limited Entry Pathways
Entry into the programme is currently through 'closed' information seminars and an assessment of qualifications. This closed approach to applications and lack of transparency may limit the chances for many candidates, especially those who may have difficulty reaching the specific venues where the information sessions are held.
Intense Time Commitment, Stress & Potential Burnout
While the apprenticeship offers the benefit of earning while learning, there are concerns regarding the workload, as the programme demands an exceedingly intense time commitment with almost no free time. Studying medicine is hard enough on its own, but adding more responsibilities can lead to a significant impact on work-life balance, potentially resulting in burnout and increased stress levels among participants.
Apprentices will need to manage intense schedules to balance their responsibilities within the NHS alongside their academic study, which could negatively affect their well-being and performance. Apprentices will need adequate support to mitigate this risk and ensure they succeed in both their training and healthcare roles.
Currently, there’s no information available about support services associated with apprenticeship positions.
Training Quality and Consistency
There is no guarantee that the quality and consistency of training will be the same for each apprentice. The educational experience, clinical exposure, and mentoring quality will vary significantly between medical schools, NHS trusts and the respective apprentice-taking doctors.
This could lead to differences in the level of preparation and competence of graduates and, subsequently, the quality of healthcare services that they will be providing. Critics of the programme have also expressed concerns about the condensed nature of the training and the lack of comprehensive theoretical study.
With the currently available apprenticeship curricula, students will completely stop having university lectures in their 4th year. This may result in gaps in knowledge and skills, which could compromise the quality of care provided by apprenticeship-trained physicians.
Potential Shortage of Training Spaces
A significant logistical challenge is the potential shortage of hospital training spaces and teaching personnel. With the NHS already stretched thin, there are concerns about whether there will be enough clinical placements for everyone.
According to the NHS workforce plan, the number of medical students is projected to double to over 15,000 by the 2030s, alongside an increase of 2,000 apprentices. However, this expansion occurs amidst stagnant speciality training numbers, with no confirmed increases aside from a planned addition of 6,000 places in general practice.
As a result, hospitals and teaching sites may struggle to provide the necessary supervision and hands-on experience that apprentices require. Addressing this issue will be crucial for the programme’s success to guarantee that all trainees can have sufficient clinical exposure to become competent practitioners.
Limited Prestige and Recognition
Another drawback of the Apprenticeship Doctor Degree is the potential lack of prestige and recognition compared to traditional medical degrees. The millennia-old traditional route of becoming a doctor is deeply rooted in and respected in the medical community around the world.
Graduates of the untested apprenticeship programme may face significant scepticism and scrutiny from patients, colleagues, and the medical community at large since it sidesteps the established path to becoming a doctor. It lacks a proven track record and a way to prove that apprentices aren’t just the students who couldn’t get accepted into a medical school.
High Workplace Pressure
The combination of academic requirements, clinical responsibilities, and the expectation to perform at a professional level can contribute to a challenging and potentially overwhelming work environment for apprentices.
Potential Long-Term Impact on the Workforce
The apprenticeship scheme is designed to bolster the NHS workforce, but it also raises questions about its long-term impact. Will this alternative route create a sustainable solution to the healthcare staffing crisis, or might it unintentionally affect the quality of future doctors?
Both the medical community and the general public worry whether the faster, earn-as-you-learn approach might sacrifice the quality of education and patient care that is ensured by traditional medical school paths.
Will Apprentices Have the Same Employment Opportunities as Traditionally Trained Doctors?
Another concern is whether apprentices will encounter stigma or limitations in career progression when compared to traditionally trained doctors. While they will graduate with the same qualifications, some in the medical community worry that this route may not be viewed as equal by employers or colleagues.
Although currently, it is alleged that an apprenticeship will hold the same value as a traditional medical degree, it is uncertain whether that will remain true. Questions also arise about whether apprentices will be able to pursue higher qualifications and specialised training or progress in the medical field.
These questions about long-term career opportunities remain largely unanswered, as the first cohort has yet to enter the workforce. For the NHS to ensure the domestic success of this alternative pathway, it must equip students with the same competencies, qualifications, and opportunities as those offered by traditional routes.
Join Our Webinar


The NHS Medical Doctor Degree Apprenticeship is making waves as a new pathway into the medical profession. Have questions or doubts about this unconventional route? Wondering how it compares to traditional medical education or if it aligns with your career goals?
We’re here to help! Join Medlink Students’ webinar, where we will break down everything you need to know about your future medical studies.
What Viable Alternatives are there to Studying Medicine in the UK?
If you are an aspiring medical student but don’t want to or can’t go to a medical school in the UK for one reason or another, there’s no need to worry. There are several GMC-approved and internationally recognised alternatives waiting for you.
The first is to study medicine in Europe. Thanks to the Bologna Process, all universities within the European Union and European Economic Area are automatically accepted by the GMC. If you want to explore options beyond the EU border, there are many top-tier universities in Eastern Europe that cover all of the GMC criteria.
When you graduate from one of these universities, all you’ll need to do is pass the UKMLA, and you’ll be ready to go back home to the UK to secure your placements.
A different path is to study in the Caribbean, which also offers a graduate entry path into medicine. The higher education system in the Caribbean is similar to that in the US in terms of quality and standards, except it has several added benefits: you won’t need to break the bank, and you’ll be studying in a tropical island paradise.
Medlink Students offers a free consultation with one of our expert academic advisors, who can guide you toward choosing the best medical school according to your goals. We’re a team of doctors and dentists with 12+ years of experience helping thousands of students just like you. We work with 100+ of the top universities in Europe and the Caribbean, where you can get a high-quality and internationally recognised medical education.
Make use of our expertise by signing up for your free consultation today and we’ll make sure that you achieve your dreams of becoming a successful doctor.
Conclusion
While the Medical Apprenticeship Programme offers an alternative pathway to entering the medical profession, it’s important to critically evaluate the long-term implications of participating in the programme.
There are still too many uncertainties with this option and while you’re guaranteed a salary from Year 1, you need to make sure that the apprenticeship aligns with your professional goals and personal well-being.
At the end of the day, why take a gamble with not just 5-6 years of your life but potentially your entire future career? Especially when you can pick a proven pathway into medicine that’s abroad, with a track record of training outstanding healthcare professionals.
Q&A Medical Apprenticeship Programme
1. What is the Medical Apprenticeship Programme?
The Medical Doctor Degree Apprenticeship provides an alternative route into medicine, allowing students to work and earn a salary while they study and train within the NHS.
2. What does the General Medical Council (GMC) say about the programme?
The GMC has not yet approved any apprenticeship programmes. Their focus remains on ensuring that all medical qualifications, including those obtained through apprenticeships, meet the required standards of quality and safety.
3. How was the Doctor Apprenticeship Programme initiated?
It was introduced in 2022 by NHS England in collaboration with Health Education England and other educational bodies to address the shortage of medical professionals by offering a paid route into the medical profession.
4. What are the entry requirements for the Medical Apprenticeship Programme?
Candidates typically need high A-level grades in science subjects, strong GCSE scores, and they must undergo an interview process. Specific requirements can vary depending on the NHS trust and university involved.
5. What does the training structure look like for apprentices?
The program lasts approximately 5-6 years, combining university coursework with practical training at NHS facilities. The curriculum gradually transitions from classroom learning to more intensive hospital placements.
6. What are the potential challenges of the Medical Apprenticeship Programme?
Challenges with the apprenticeships to become a doctor include intense time commitments, potential variability in training quality, concerns about the thoroughness of the educational experience, and issues related to the recognition and prestige of the pathway.
7. How is the programme perceived by current medical professionals?
Opinions vary significantly; while some are hopeful that it provides a solution to healthcare staffing shortages, many others are sceptical about the quality of training and the potential impact on professional standards.
8. Are there guarantees of employment upon completion of the apprenticeship?
While the programme aims to integrate apprentices into the NHS, like all medical graduates, apprentices must still meet all standard qualification requirements, including passing the UKMLA, to practise as doctors.
9. What are viable alternatives to studying medicine in the UK?
Alternatives include studying in accredited and internationally recognised universities in Europe and the Caribbean. Medlink Students can assist you in finding the perfect medical school for you that fulfils all GMC criteria.
10. How do you apply for a Medical Apprenticeship Programme?
Currently, applications for the Medical Degree Apprenticeship programme are made through ‘closed information seminars’ at select locations. Prospective candidates will be assessed at this seminar and may be invited to participate.
4 comments on “NHS Medical Doctor Degree Apprenticeship - All Facts in 1 Place”
Leave a Reply
About Medlink Students
Leading international recruitment company for medical students in Europe. British Council Certified Agents. 10+ years of experience and more than 10,000 students advised.









I would like my daughter to be supported to get a place
I want free advice
I want advice regarding medical doctor
Hello,how do I apply for a medical apprientiship degre ? When I want to start in September 2026 next year