MMI Interview Questions: Complete Guide for Medical School Interview Success


You’ve spent months preparing for medical school, studying diligently and acing all your exams. Now, there’s just one hurdle left: the dreaded bombardment of questions, a.k.a. the interview.
But most medical schools have shifted away from using the old school interview format, where a panel of professors fire off rapid-fire questions at you. Instead, prospective medical students should expect a circuit of mini “stations,” where they tackle everything from moral dilemmas to role-play situations with an actor. Each of these sections lasts just a few minutes, and the whole circuit is formally called Multiple Mini Interviews, or MMI for short.
Nowadays, this is 1 of the most common medical school interview formats and is something every student should be prepared for. In this blog, we will break down the MMI structure by going through what each station tests with example questions, answers, tips, and much more.
The key takeaways of this blog include:
- The Multiple Mini Interview consists of 6-10 short stations, where candidates are tested on various skills such as communication, ethics, problem-solving, and empathy.
- Each station lasts 5-8 minutes with a fixed time for thinking and responding.
- MMIs offer a more objective and reliable way to assess candidates, focusing on real-world skills like patient communication, ethical judgment, and decision-making under pressure.
- MMIs are scored based on station-specific rubrics, assessing attributes like communication, professionalism, and ethical reasoning.
- The main MMI station types include ethical dilemmas, role-play scenarios, situational judgment, teamwork, and personal reflection.
- Each station tests different core skills important for a future doctor, such as empathy, critical thinking, and leadership.
Table of Contents
- 1 Part 1: The MMI Structure
- 2 Full MMI Interview Stations Breakdown
- 3 Part 2: Sample MMI Interview With Answers
- 4 Part 3: Now It’s Your Turn to Take an MMI
- 5 The MMI Prep Checklist With Tips
- 6 Why This Matters to You
- 7 Q&A: MMI Interview Questions
- 7.1 What should I do if I’m unsure about a question in an MMI?
- 7.2 How are MMI stations scored?
- 7.3 What is the best way to prepare for role-play stations?
- 7.4 How do I handle the pressure of an MMI station?
- 7.5 How important is ethical reasoning in the MMI?
- 7.6 Can I get feedback after the MMI?
- 7.7 How do I manage time during an MMI?
Part 1: The MMI Structure
An MMI is a circuit of short, timed stations, usually between 6 and 10 in total. At each station, you will receive a prompt, task or question in the form of a written scenario, a role-play script or a group task brief.
You will then be given a fixed time, often between 5-8 minutes, to read, think and respond. Meanwhile, a dedicated station assessor (or 2) will be observing your performance, using a set of rules to score you. This format ensures that no single question makes or breaks your interview; instead, you can demonstrate a consistent range of skills across varied challenges.
After each station’s buzzer, you’ll have a brief transition period to move to the next room (typically 1–2 minutes). Some circuits even include a rest station, a quiet room where you sit out for 1 round. Make sure to use this pause to breathe, re-centre and glance at a quick “cheat-sheet” of frameworks or buzzwords, like SPIKES for breaking bad news or STAR for personal questions (more details further in the blog).
A quick piece of advice from us is to try to familiarise yourself with the building layout in advance. If possible, arrive early to scout out the room numbers and corridor routes, so you won’t stress over where you need to head next.
Why Do Medical Schools Use the MMI?
The MMI medical interview has steadily been replacing panel interviews because it offers a more reliable and comprehensive way to assess a candidate's suitability for medical school. They give an objective overview of who you are as a candidate and how you’ll perform as a future doctor.
The most significant advantages include:
- Improved reliability. Multiple stations mean 1 tricky question won’t decide the outcome of your interview.
- Reduced bias, thanks to the variety of examiners at each station.
- Real-world skills testing that includes patient communication, making ethical judgments, and handling specific cases from the day-to-day demands of clinical practice.
- Interview standardisation, where every candidate faces the same scenarios under identical conditions, making comparisons fairer and easier to asses.
How MMI Differs from Traditional Panel Interviews
Traditional interviews depend on your performance in 1 extended conversation. This often means that having nerves, facing 1 difficult question that interrupts your thought process, or a subjective panel dynamic can tilt the outcome against you.
Medical MMIs, by contrast, spread the risk and reward across many bite-sized interactions, giving you more opportunities to shine, where a “wrong” answer doesn’t spell the end of your prospects.
In a nutshell, the main differences are:
| Panel interview | Multiple Mini Interview (MMI) | |
| Format | One or two panels of 3–5 interviewers | 6–10 short stations with rotating assessors |
| Question Style | Broad, often unpredictable | Focused prompts with clear objectives |
| Duration | 20–60 minutes of continuous interview | 5–8 minutes per station, with breaks |
| Assessment | Overview with a holistic impression | Station-specific scoring rubrics |
| Bias Mitigation | Single or dual perspectives | Multiple examiners across stations |
| Feedback Potential | Rarely standardised, often decided by the interviewer's discretion | Each station is scored independently |
How are MMIs Scored?
Examiners use detailed score sheets with station-specific rubrics that break down each station into discrete criteria like clarity of communication, ethical reasoning, empathy, etc. In addition to ticking off checklist items, many rubrics include a global rating, e.g. “Excellent,” “Competent,” “Needs Improvement”, to capture your overall impression.
Some schools employ single marking, where 1 assessor scores your performance, but many also use double marking, with 2 examiners independently scoring the same station to increase reliability. So don’t get stressed out if there’s more than 1 examiner all of a sudden.
As far as feedback goes, you shouldn’t expect detailed station-by-station feedback. Examiners’ written comments are considered confidential and are not typically shared with candidates. Instead, you’ll either receive a pass/fail outcome or a score to show how well you did out of 100.
Full MMI Interview Stations Breakdown
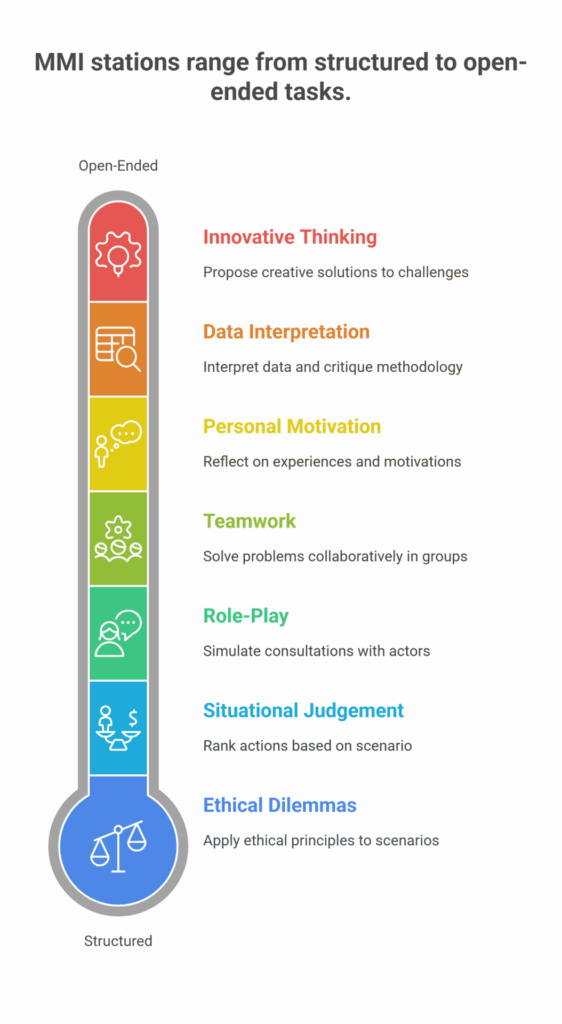
MMI stations come in a variety of formats, each designed to test a different aspect of your suitability for medicine. Below is a rundown of the most common station types, with notes on how they’re set up and exactly what skills or attributes you’ll be demonstrating.
We will give you a quick overview of each station, along with what skills you are being tested for. Right after this, we will follow up with a quick quiz with actual questions from MMI interviews and their proper responses.
Here’s a rundown of the most common MMI question types, including medical MMI questions, medical ethics MMI questions, and role-play scenarios:
Ethical Dilemmas
Typically, at this station, you will be presented with a short written scenario describing an ethical conundrum, ranging from confidential information sharing to dealing with a witnessed malpractice and more. You’ll usually have 1–2 minutes to read, then 5–8 minutes to discuss your approach with an assessor.
Important skills and attributes here are your knowledge of professional guidelines, ethical reasoning, moral judgement and ability to balance competing patient interests.
Your best approach to the ethics MMI questions is to make use of the 5 pillars of medical ethics:
- Autonomy - respecting a patient’s right to make their own informed decisions about treatment after your input/guidance.
- Beneficence - acting in the best interests of the patient to promote their welfare.
- Non-maleficence - avoiding harm or minimising risk to the patient whenever possible.
- Justice - ensuring fair distribution of healthcare resources and treating patients equally and equitably.
- Confidentiality - safeguarding patient information and only sharing it with appropriate consent or legal justification.
A great read-through for any future doctor would be to go over the General Medical Council’s (GMC) Good Medical Practice guidelines.
Situational Judgement and Problem-Solving
At this station, you will usually be given a list of possible actions or responses to a practical scenario in either a written or oral format. You’ll then be asked to rank, choose, or justify the best and worst options in this scenario, as is typical of MMI medical interview prompts.
Here’s an example - several patients are waiting in line at your GP surgery:
- A 10-year-old with a high fever and stiff neck
- A diabetic with a non-healing foot ulcer
- An elderly patient due for a routine blood-pressure check
Your possible actions are:
- See the child with suspected meningitis immediately
- Ask the elderly patient to come back later in the afternoon
- Triage all patients with a nurse and reprioritise
- Stick to the appointment schedule and see each in turn
- Call a senior GP for advice on managing the diabetic’s ulcer
You’ll be asked to pick or rank the best and worst choices and explain your reasoning.
The important skills and attributes for this section are analytical reasoning and decision making under pressure with justifiable prioritisation through awareness of policies and/or protocols.
The best approach for this section is to read the question twice and make sure to scan the scenario for the facts and criteria that will help you form a decision. Consider whether patient safety, confidentiality, or fairness are the deciding factors and vocalise your reasoning leading up to your judgment.
To really hit the ball out of the park, anchor to guidelines or protocols. For example, you can say that “According to the British Medical Association’s triage protocols, initial sorting by severity helps allocate resources where they’re needed most. This ensures every patient is assessed for urgency, maximising safety and efficiency. In this situation, I would triage all patients and prioritise the at-risk child. I would rank the answers C), A), B), E), D).”
Role-Play Stations
In this station, you will interact with a trained actor who plays the role of a patient, relative, or colleague. You will be given a brief “prompt card” that outlines the scenario, after which you will be given a few minutes to conduct the simulated consultation. In MMI interviews for medicine, role-play scenarios are very common.
An example scenario could be that the actor plays Mr Patel, a 55-year-old man recently diagnosed with stage 2 hypertension. He’s worried about starting lifelong medication and asks if lifestyle changes alone might be enough.
The skills and attributes assessed here are verbal and nonverbal communication, empathy, rapport building, professionalism, and boundary setting. Examiners will watch how you open the conversation, respond to emotions, explain medical information clearly, and close with a plan.
The best approach is to structure your mini-consultation according to the Calgary-Cambridge model or the SPIKES protocol for breaking bad news. Start with an open-ended question, acknowledge the actor’s feelings - “I understand this can feel overwhelming.” Anchor your language to GMC Good Medical Practice - “I’m here to support you and give you the information you need to decide”. Then check for understanding - “Can you tell me what you think about your options?” and end by summarising next steps based on your patient's best interests.
Teamwork / Collaboration Exercises


For this station, you will be presented with a small-group task (typically 3 to 5 candidates) with a time-limited problem to solve together, e.g. ranking priorities for a new medical practice or designing a simple intervention.
An example situation would be designing an outreach initiative to boost vaccination rates in a vaccine-hesitant community. You are given 5-10 minutes to collaborate, agree on a strategy and present your plan.
The skills and attributes that are being tested here are leadership, active listening, negotiation skills, clear communication, ability to compromise, respect for different opinions and conflict resolution.
The best approach for this station and similar scenarios is to start with a quick round-robin so everyone shares 1 idea. Then follow up by establishing clear criteria, like which element would increase public trust the most? Remember to invite quieter members to contribute, and keep track of time. Summarise the options and, if time allows, rank them before presenting your final decision.
Personal Motivation & Reflection
A 1-to-1 station where you answer questions about yourself, like why you want to study medicine, how you handle stress, or lessons learned from past experiences.
An example question would be “What made you decide to pursue medicine as a career?”
The important skills and attributes in this section are self-awareness and insight with the ability to verbally demonstrate resilience, adaptability, genuine motivation and long-term commitment.
The best approach here is to structure your answer using the STAR method:
- Situation and Task. Set the scene and give clear details on what personally motivated you.
- Action. Describe what you did, how and why in order to get started on this path. For example, volunteering or shadowing a doctor.
- Result. Share the outcome, what you learned from it and how it has helped you.
Choose a concise, meaningful example, speak honestly, and always link your experience back to how it shapes you as a future doctor.
The perfect read to completely prepare you for this MMI interview for medicine is our blog on: Why Study Medicine? A Comprehensive Guide to Help You Decide & Ace Interviews
Data Interpretation & Research
In this station, you’ll be provided with graphs, tables or a brief research abstract. Your task is to interpret the data, identify trends or anomalies, and critique the methodology. After which you’ll discuss your findings with the assessor.
For example, you’re given a table displaying the average waiting times for GP appointments in different areas of the city over the past 12 months. Your job is to identify trends, potential causes for discrepancies between regions, and suggest improvements.
Useful skills and attributes here are numeracy & data literacy, critical appraisal of evidence and the ability to communicate complex information clearly.
The best approach at this station is to quickly identify patterns or outliers and discuss their significance. For instance, if 1 region has notably longer waiting times, consider the factors that could contribute, such as staffing shortages or increased patient demand.
Critique the methodology where applicable, like the sample size or data collection method, and suggest practical solutions for improvement based on your findings. Always present your thoughts in a clear, logical sequence, making sure your reasoning is easy to follow.
Innovative and Creative Thinking (Optional)
At this station, you will typically be presented with an open-ended prompt, such as redesigning a hospital waiting room or conceptualising a new public health campaign. These tasks assess your ability to think creatively and propose practical solutions to unorthodox challenges. You might be encouraged to present your ideas verbally or even sketch them out.
An example here could be redesigning a new hospital waiting room that enhances patient comfort and reduces anxiety.
The skills and attributes being tested here are originality, outside-the-box thinking, flexibility, adaptability and being able to propose practical solutions to unorthodox situations.
The best approach for this section is to start by fully understanding the problem and identifying key challenges. “Why is the waiting room being redesigned, and what’s wrong with it?” Brainstorm a range of creative ideas that address the issues, ensuring they are both practical and feasible.
Evaluate the pros and cons of each solution, considering factors like cost, feasibility, and patient impact. Present your ideas clearly, using simple language and visual aids if possible, and always link your solutions to core healthcare principles like patient care, efficiency, and accessibility.
Part 2: Sample MMI Interview With Answers
Note: These scenarios are inspired by real MMI prompts but are illustrative rather than taken verbatim.
Station 1: Ethical Dilemma
Situation: you witnessed a fellow student cheating on a university exam. What do you do?
What assessors will be looking for: honesty, responsibility, awareness of GMC Good Medical Practice
Example approach:
1. Reflect on the seriousness of the accusation and acknowledge the impact on fairness and future patient safety. You could say, “Academic integrity is vital to public trust in doctors.”
2. Formulate an action plan, like speaking privately to your peer first to give them a chance to explain, correct their behaviour and take responsibility. Escalate to the faculty or the exam board if the issue remains unresolved.
3. Finally, reference professional guidelines to justify your decision. “According to GMC Good Medical Practice standards, I have a duty to raise concerns to protect standards and patient welfare.”
Station 2: Role-Play. Delivering Bad News
Situation: an actor is playing Mrs Smith, a parent whose child has just been diagnosed with Type 1 diabetes.
What you’re being tested for: empathy, clear explanation, checking understanding, offering support and solutions.
Example answer:
1. Start with an introduction and rapport by saying, “Good afternoon, Mrs. Smith. I’m Dr. Johnson, and it’s a pleasure to meet you. Thank you for coming in today.”
2. Deliver the news in plain language: “The tests show that James’s pancreas isn’t producing enough insulin, a sign of Type 1 diabetes. This means his body isn’t able to process sugar properly, but we can manage it effectively.”
3. Pause and allow reaction. Give Mrs Smith time to process the information. Pay attention to her non-verbal cues and provide a supportive presence.
4. Offer reassurance, “I can understand how overwhelming this must be for you, but there’s no need to worry. Type 1 diabetes is completely manageable with the right care, and we’re here to help you and James every step of the way.”
5. Answer any questions & outline the next steps. Be prepared to answer any immediate questions. Clearly outline what happens next: “The next steps involve insulin training for you and James, and we’ll also work together on a diet plan. We’ll have a follow-up appointment in 2 days to make sure everything’s going smoothly.”
6. Offer additional support & resources, “I know this is a lot to absorb right now, so we have a diabetes nurse specialist who will meet with you tomorrow to go over everything in more detail. Additionally, here’s a leaflet with resources and contact details for further support.”
Station 3: Teamwork Exercise
Situation: in a group of 4, rank the 5 public health priorities for your new GP practice within 10 minutes.
What’s expected: leadership, listening, compromise, and time management
Example approach:
1. Make a quick round-robin with suggestions, “Let’s go around and share 1 priority each, so everyone’s view is heard.”
2. Propose criteria to help you rank priorities, “Shall we decide based on which issue most affects patient safety or community need?”
3. Summarise & build consensus. “It looks like we’re all leaning towards mental health support as a top priority. Would we all agree that tackling mental health problems in our community should be our focus? What do we think about addressing obesity or diabetes as the next issue?”
4. Keep on track by using time checks: “3 minutes left, let’s confirm our top 5 now.”
Station 4: Situational Judgement
Situation: rank the following actions if a colleague is frequently late for on-calls:
- Report to your supervisor
- Talk to them privately
- Ignore
- Offer a flexible rota
What assessors are looking for: professionalism, problem-solving, and patient-safety awareness.
Example answer: B), D), A), C)
“First, I would talk privately with my colleague to understand their reasons and offer support before taking further steps. Then, I would offer a flexible rota to solve the problem by adjusting shifts if needed. If that proves unsuccessful, I would escalate and report to my supervisor if lateness persists and affects patient care. I would never ignore the issue as it affects patient safety, team morale, and the standing of our establishment.
Station 5: Personal Motivation
Prompt: give an example about a time you overcame a significant challenge.
What attributes they’re looking for: resilience, reflection, and a growth mindset
Example response structure using STAR:
- Situation: “In my second year, I juggled part-time work with a demanding lab project.”
- Task: “I needed to deliver my project on time while covering shifts.”
- Action: “I created a strict study schedule, negotiated fewer shifts, and joined a peer-support study group.”
- Result: “I submitted the project 2 days early with high marks, and learned invaluable time-management skills.”
Station 6: Data Interpretation
Task: you’re given a graph showing vaccination uptake in 2 regions over 5 years. Identify trends and suggest potential causes.
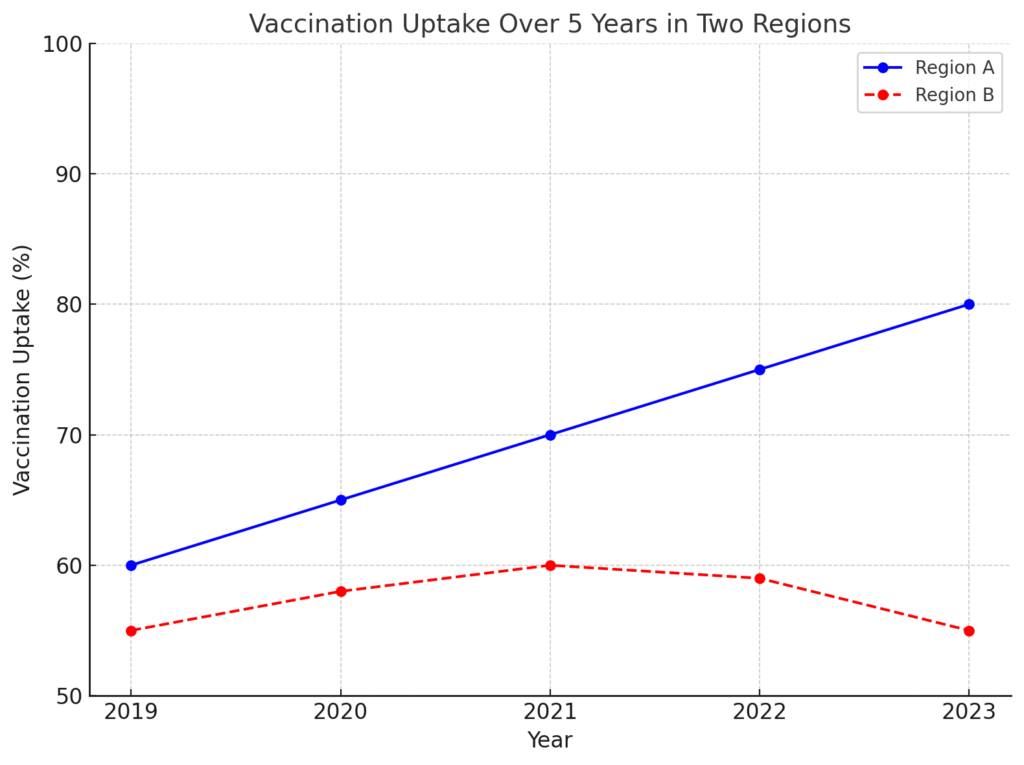
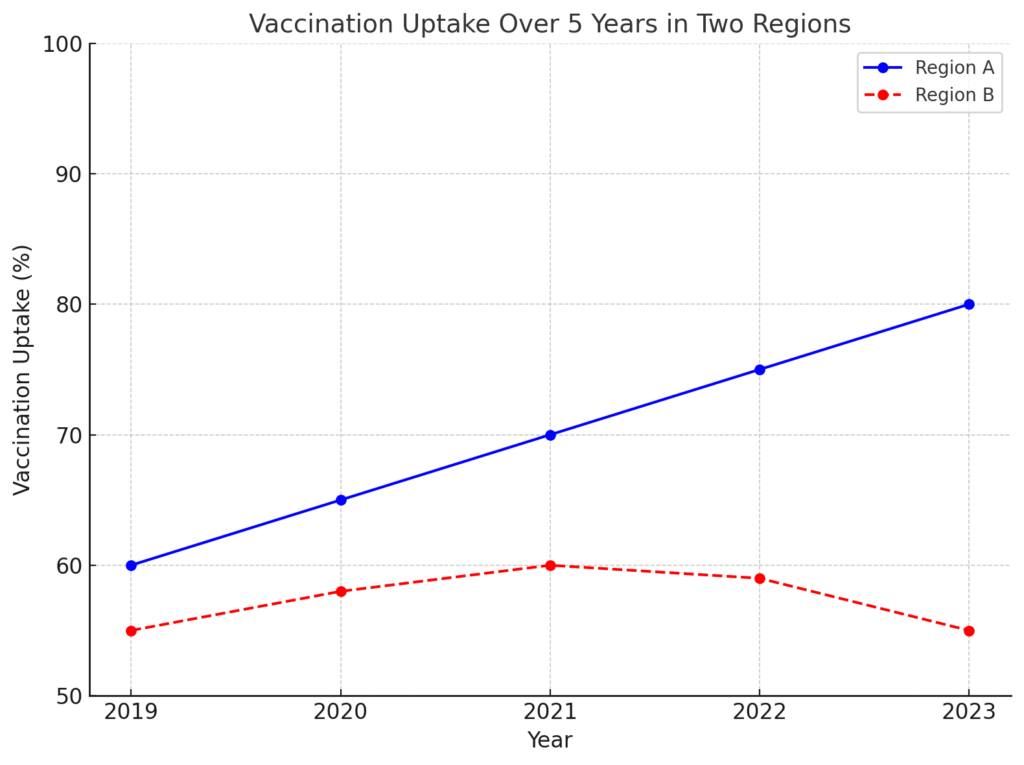
Skills you’re being tested for: numeracy, critical thinking, and public health awareness.
Example answer:
1. Identify the trends. "Region A shows a steady increase in vaccination uptake over the five years, rising from 60% to 80%. In contrast, Region B shows fluctuations, with a slight decline from 60% to 55% in the last 2 years."
2. If allowed, ask follow-up questions. “Were there any supply shortages or changes in eligibility criteria?”
3. Suggest Potential causes: "The increase in Region A could be due to successful public health campaigns or improved access to vaccines. The decline in Region B may be attributed to factors such as vaccine hesitancy, misinformation, or reduced local health services."
4. Offer suggestions. "To improve uptake in Region B, targeted outreach, community education, and addressing misinformation could help reverse the downward trend. We can introduce community outreach programmes and partner with local clinics to boost trust.”
Section 7: Creativity
Situation: you’ve been tasked with designing a new mobile healthcare app specifically for elderly patients. The app should help them manage their medications, track doctors’ appointments, and offer support for general health. How would you approach this task?
What you’re being tested for: creativity, practical problem-solving, accessibility, and technology integration.
Example answer: “To design a user-friendly app for elderly patients, I’d focus on simplicity with large buttons and clear navigation. Key features would include medication reminders, an appointment calendar, and a daily health checklist. Accessibility features like adjustable text size and high contrast visuals should be integrated for those with limited tech skills or visual impairments. If the resources allow, voice commands would be an excellent but costly integration. Instead, we can offer tutorials and live with the option for family members to monitor progress.”
Part 3: Now It’s Your Turn to Take an MMI
Give yourself 5–8 minutes per scenario, then pause and jot down your response before checking model outlines.
Station 1: Ethical Dilemma
You overhear a nurse using unprofessional language about a patient in the corridor. How would you handle it?
Station 2: Role-Play. Breaking Bad News
The actor plays a 50-year-old patient who’s just tested positive for early-stage cancer. How would you approach this conversation?
Station 3: Teamwork Exercise
In a group of four, devise a plan to reduce waiting times in a busy A&E department. Rank your top three strategies in 10 minutes.
Station 4: Situational Judgement
Rank these actions if you suspect a colleague is not washing their hands between patient contacts:
- Ignore it
- Offer a gentle reminder
- Report to the supervisor
- Model proper technique publicly
Station 5: Personal Motivation
Describe a time when you failed at something important and how you bounced back.
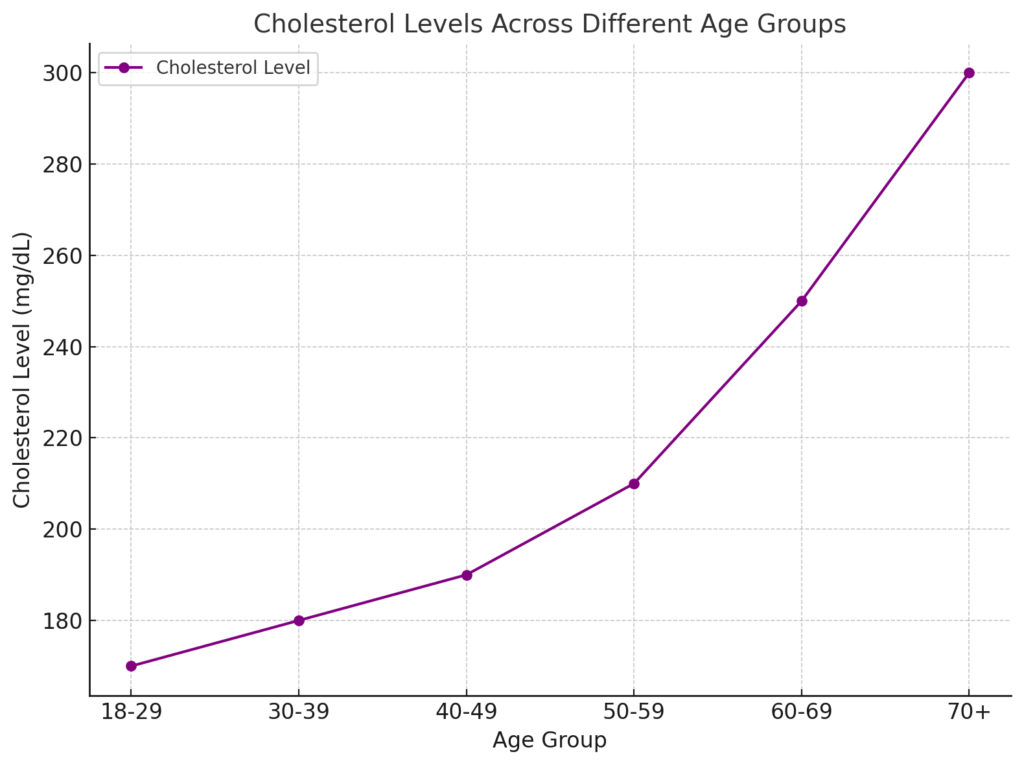
Station 6: Data Interpretation
You are provided with the following data showing cholesterol levels across different age groups. Identify any trends or outliers in the data and suggest what further information you would request to better understand these trends. Explain what the reasons could be for these outliers.
Station 7: Creativity
Design a public health campaign to reduce smoking among teenagers in your community. What would be the key elements of your campaign, and how would you ensure its success?
The MMI Prep Checklist With Tips
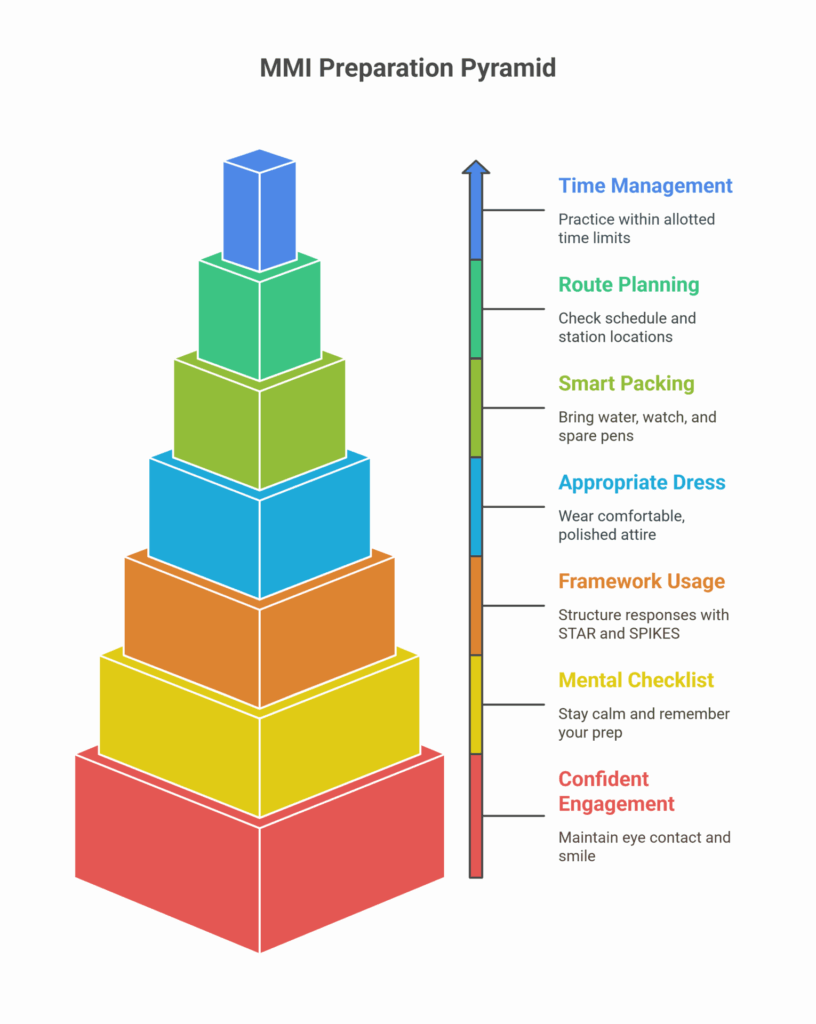
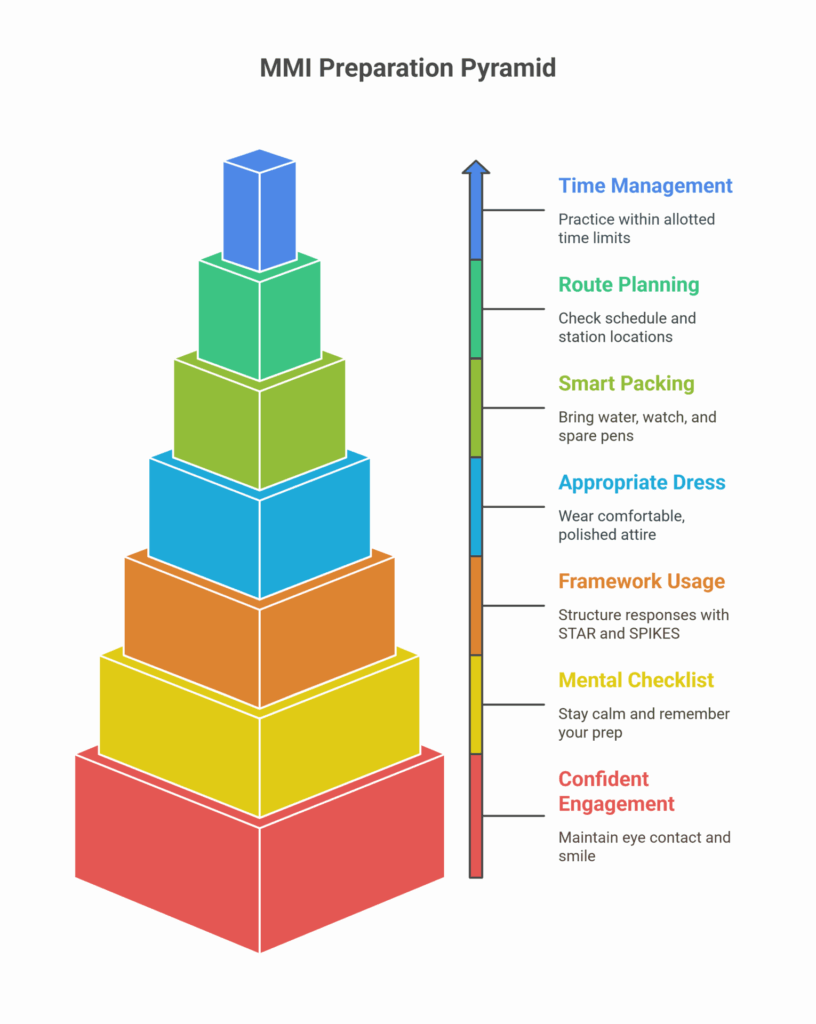
- Time your practice when running through mock stations at home or with peers. Using a stopwatch or phone timer, aim to hit your main points within the allotted 5 to 8 minutes.
- Plan your route by checking the interview day schedule and station locations. A quick tip is also to note the nearest bathrooms and water stations so you’re always calm, cool and collected.
- Pack smart and bring a clear plastic bottle of water, a wristwatch (if allowed) and spare pens. Keep your phone off and tucked away to avoid accidental distractions.
- Dress appropriately and opt for smart, comfortable attire and shoes. Whether you’re taking an online MMI or in-person, you’ll want to look polished without feeling stiff.
- Use frameworks like STAR and SPIKES to structure responses.
- Perform a quick mental checklist before each station. Stay calm, breathe and remember your prep to formulate your answer: “First, I’ll clarify X, then I’ll go over Y, and use the Z protocol to justify my decision.”
Engage with direct eye contact and a confident smile. Remember that examiners want to see you at your best.
Why This Matters to You
Your performance in each MMI station is much more than an academic exercise. It’s a window into how you’ll handle real clinical challenges from day 1.
A single mistake, like failing to spot an ethical conflict or hesitating under pressure in a role-play, can leave assessors questioning your readiness for medicine. Unprepared candidates risk lower scores, missed interview offers, and even the worst-case scenario, not getting accepted into medical school.
But you don’t have to stress out and prepare for it alone. The Medlink Students Student Success Programme is designed to prepare you to ace any medical school interview, entrance exam, and much more. From mock exams modelled on real interviews to ongoing support right up to the big day, we'll be there every step of the way.
With our expert guidance, you’ll enter each MMI station not just ready, but with confidence.
Q&A: MMI Interview Questions
What should I do if I’m unsure about a question in an MMI?
If you're unsure how to handle a specific MMI medical interview question, it’s okay to ask for clarification, but don’t over-explain the issue. Take a moment to structure your thoughts, stay calm, and demonstrate your problem-solving and communication skills.
How are MMI stations scored?
MMI stations are typically scored on a detailed rubric, assessing your performance on specific criteria like clarity of communication, ethical reasoning, and professionalism. Examiners may give a global rating, such as “Excellent” or “Needs Improvement.”
What is the best way to prepare for role-play stations?
For role-play stations, focus on active listening, empathy, and communication. Practice responding to emotional scenarios, explaining complex concepts simply, and summarising next steps clearly. Use frameworks like Calgary-Cambridge or SPIKES.
How do I handle the pressure of an MMI station?
Practice makes perfect. If you’re well-prepared, the pressure on you will be significantly lower. Once you’re actually at the station, stay calm, breathe, and remember that each station is short, so you have limited time to make a good impression. Use your practice to quickly think through the question, structure your response, and remain confident.
How important is ethical reasoning in the MMI?
Ethical reasoning is crucial, as many stations are designed to test your ability to make decisions with patient welfare in mind. Use the 5 pillars of medical ethics (autonomy, beneficence, non-maleficence, justice, and confidentiality) to guide your responses.
Can I get feedback after the MMI?
Detailed feedback is rarely provided on individual stations, as it is considered confidential information. Most schools will give you a pass/fail outcome or an overall score.
How do I manage time during an MMI?
Practice with timers to ensure you can hit your key points within the allocated time. Ensure you’re aware of the time at each station. You typically have 5-8 minutes per station, so structure your responses efficiently.
Leave a Reply
About Medlink Students
Leading international recruitment company for medical students in Europe. British Council Certified Agents. 10+ years of experience and more than 10,000 students advised.